Most dental implant stories don’t start with a big decision. They start with a small annoyance that keeps returning.
You bite into something and realise you’ve been avoiding that side for weeks. You catch yourself smiling with a slight edit — lips together, head turned, angle chosen. You realise you’ve become the person who “just doesn’t eat crusty bread anymore,” not because you don’t like it, but because it’s easier than dealing with the awkwardness.
Then you do what everyone does: You Google. And suddenly it’s all either “life-changing in one visit” or “brace for impact.” Neither of those versions feels like real life.
So this is the real-life version — the human one — where implants are explained in the way people actually need when they’re sitting at home thinking, Is this worth it? Will it be a nightmare? Am I going to regret spending the money?
The strange thing about missing a tooth: You adapt… then you get tired
At first, people are surprisingly good at adapting. You find a workaround and keep going. That’s what humans do.
But it’s the constant micro-adjustments that wear you down:
Chewing a bit carefully so food doesn’t get trapped in that spot
Swallowing slightly differently
Being hyper-aware of your tongue
Laughing with a “managed” smile
Talking and wondering if anyone can tell
If you’ve been living with a gap for a while, you might not even realise how much effort is going into the compensation. The goal of an implant, when it’s the right choice, is to remove the need for all that background managing.
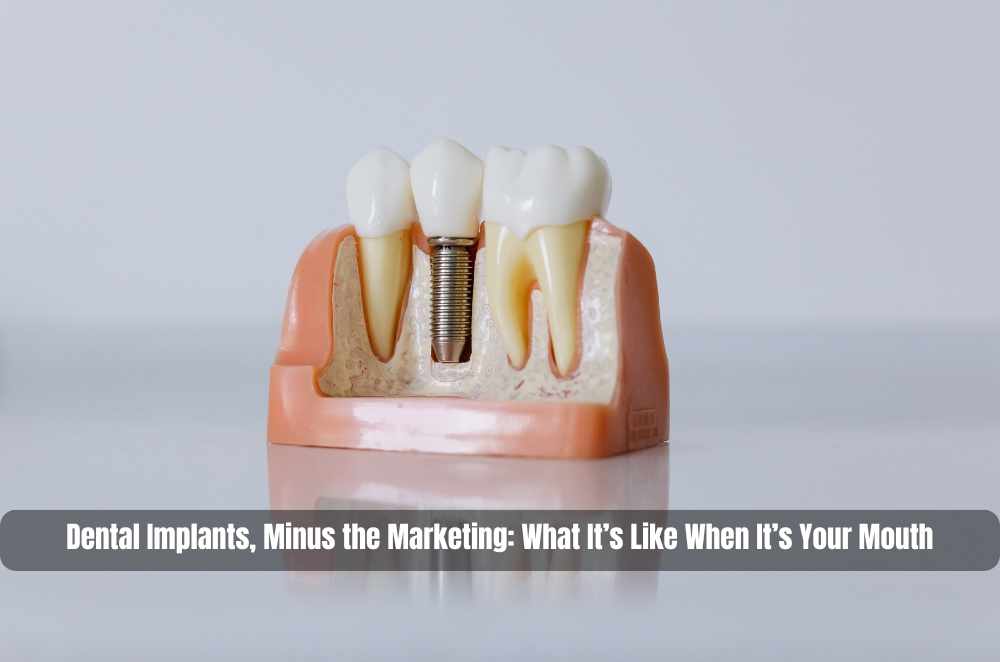
What a dental implant is — without the clinical voice
A dental implant is a small post placed into the jawbone to act like an artificial tooth root. Once it heals and bonds with the bone, it can support a replacement tooth (typically a crown). In other situations, implants can support multiple teeth or larger restorations.
That’s the plain-language version: it’s a foundation first, a tooth second.
And that’s why people often describe implants as feeling more “part of them” than some other replacements — because they’re anchored where a root used to be, rather than sitting on top of the gums or leaning on neighbouring teeth.
The question behind the question: “Will my mouth actually accept this?”
This is where implant decisions become personal.
Because implants aren’t like buying a pair of glasses, where you can just swap frames. They involve your bone, your gums, your healing, and your habits. Suitability is less about being a “good patient” and more about having the right conditions.
Clinicians usually consider:
Bone support: You need enough healthy bone where the implant will sit.
Gum health: Gum disease or inflammation needs to be managed first.
Healing factors: Smoking and certain medical issues can affect healing and long-term stability.
The good news is that “not ready today” doesn’t always mean “not possible.” Sometimes it means a staged plan. What matters is that the explanation makes sense and isn’t rushed.
What the process is like when you’re the one doing it
People think implants are one dramatic event. In reality, they’re more like a series of steps with waiting in between — and the waiting is where most of the success lives.
Step 1: The planning appointment (where your future self is protected)
This is the part that can feel slow, but it’s also the part that prevents expensive regret.
A good planning conversation doesn’t just focus on the missing tooth. It looks at the whole environment: bite, spacing, gum condition, adjacent teeth, and how you actually use your mouth. It’s also where you talk about your expectations — and this matters. “Natural-looking” means different things to different people. So does “comfortable.” So does “I don’t want to think about it.”
Step 2: Implant placement (the part people fear the most)
This is when the implant is placed in the jawbone.
Here’s the honest human truth: the fear is often louder than the recovery. Not always — experiences vary — but many people report that once they know what’s normal (swelling, tenderness, eating changes), it’s far less mysterious.
This is the stage where it helps to ask practical questions, not just medical ones:
What will I be eating for the first few days?
Do I need time off work?
How do I keep it clean without aggravating it?
Clear expectations calm the nervous system. Vague reassurance does not.
Step 3: Healing and integration (the oddly frustrating middle)
After placement, the implant needs time to integrate with the bone. This is where people sometimes feel impatient because you’ve “done the thing,” but you’re not finished.
It can be mentally annoying in a quiet way — like waiting for paint to dry when you’re desperate to put the furniture back. But it’s also what makes implants stable long term. Your body is doing the work that turns “a post in bone” into “a foundation that can handle chewing.”
Step 4: The final tooth (when you stop thinking about it)
Once healing is complete, the visible tooth (often a crown) is attached.
People expect an emotional moment. What they often get is something simpler: normality.
The real sign it’s gone well isn’t that you’re thrilled. It’s that you forget about it. You eat without planning. You smile without checking. You stop doing the tiny compensations you’d been doing for months or years.
Implants vs bridges vs dentures — what people actually weigh up
Online comparisons usually read like a scoreboard. Real decisions are more like: What will annoy me the least for the next ten years?
People tend to compare:
Stability: Fixed (implant) versus removable (denture).
Impact on nearby teeth: Some options involve neighbouring teeth more than others.
Cleaning reality: What can you realistically maintain on your most exhausted days?
Timeline and tolerance: Are you okay with a staged process and healing time?
There isn’t a universally “right” choice. There is only the right match for your mouth, your health, your timeline, and your preferences.
A sensible place to start if you’re still deciding
If you want a single, straightforward overview to ground your research (so you’re not piecing together ten conflicting opinions), you can start with this explainer on the implant process and what it involves: Dental implant treatment overview (Blue Mountains Dental & Implant Centre).
Key Takeaways
Missing a tooth often affects daily life through small, ongoing adjustments that add up.
Dental implants are designed to replace the root support and the visible tooth.
Suitability depends on bone support, gum health, and healing factors — it’s individual.
The implant process is staged, and the healing phase is a key part of long-term stability.
The “best” choice is the one that fits your life and maintenance habits, not the one that sounds most impressive.









Write a comment ...